Live-in care

Our trusted live-in care service provides 24/7 support from qualified carers in your own home. Ideal for elderly individuals needing full-time dementia, Parkinson’s, or mobility support.

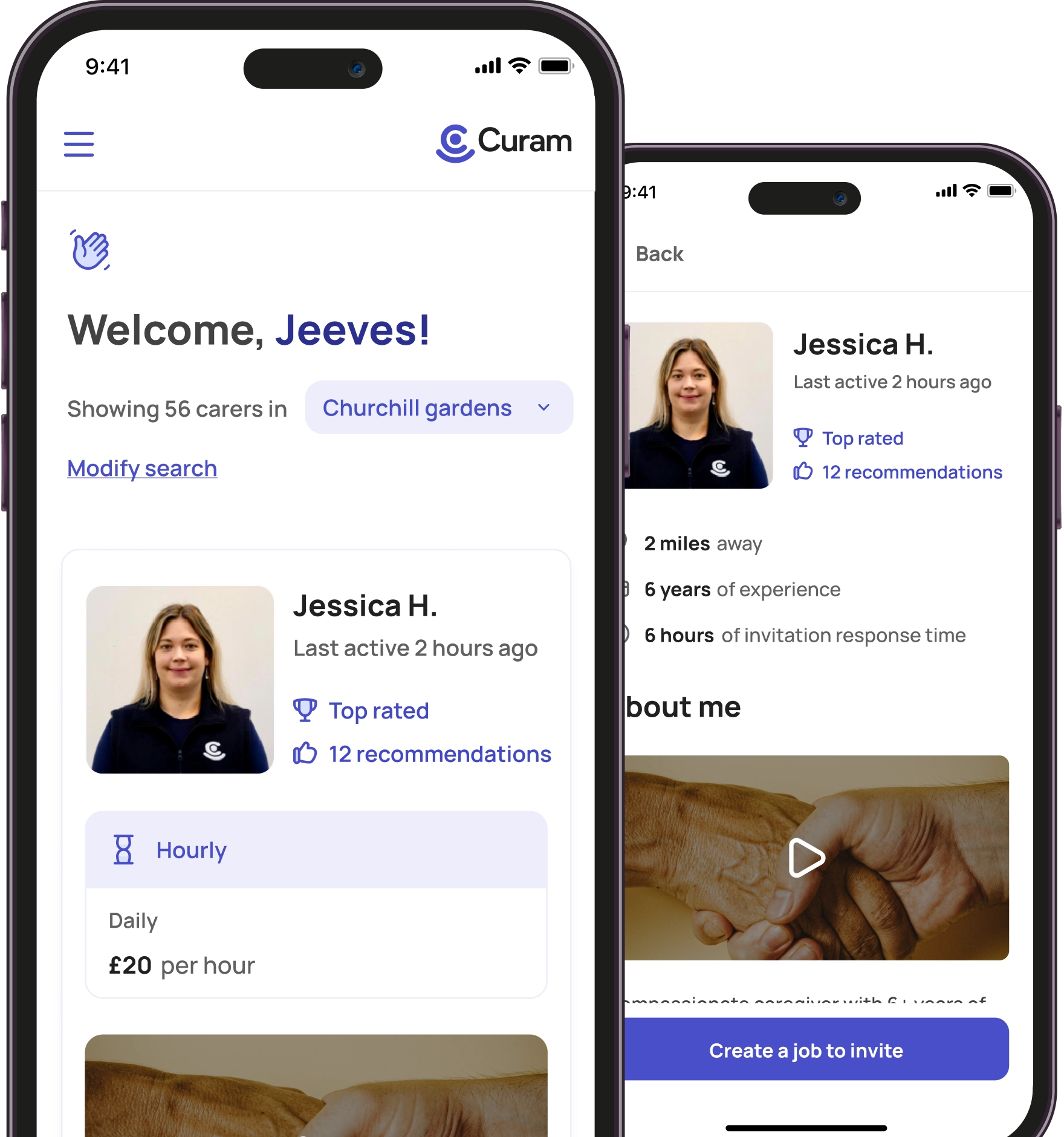
Hourly care

Flexible hourly home care tailored to your schedule. Our expert carers assist with daily tasks, medication, and companionship for seniors with early-stage conditions.

Overnight care

Overnight home care for peace of mind while your loved one sleeps. Perfect for fall prevention, personal care, and dementia-related nighttime support.

Managed care

Experience peace of mind with our CQC regulated Managed Care service. We provide expert support to help you find the right self-employed carer, with guidance, oversight, and continuity of care.
Dementia care

Expert dementia carers providing compassionate support for independence and safety at home.
Autism care

Personalised autism care at home, delivered by expert carers, supporting safety, independence, and peace of mind.
Respite care

Respite carers provide flexible home care, allowing family carers to take a break while loved ones receive ongoing support and safety.
Elderly care

Personalised elderly care at home, tailored to your unique needs for comfort, safety, and independence.
Children’s care

Customised children’s home care, delivered by trusted carers to support your child’s physical, emotional, and social development in the comfort of your home.
Post operative care

Post-operative care at home from experienced carers to support recovery, improve mobility, and restore independence after surgery.
24 hr care at home

24/7 care at home, delivered by a team of Curam carers to ensure continuous, round-the-clock support for your needs.
Domiciliary Care

Flexible home visits that support personal care, medication, mobility and daily routines—helping you stay independent at home.
How much does live-in care cost?
Explore the cost of live-in care with private carers across the UK. Learn what’s included in daily rates, how pricing compares to care homes, and how to arrange affordable, full-time home support.
How much does hourly care cost?
Find out the average hourly rates for private carers in the UK. Understand what affects the cost of part-time home care and how to choose flexible support tailored to your schedule.
How much does overnight care cost?
Get clear guidance on the cost of overnight care with private carers across the UK. Learn when night-time support is needed, how much it typically costs, and what’s included.
Calculate your home care costs across the UK
Use our care cost calculator to estimate the price of live-in, hourly, or overnight care with private carers anywhere in the UK.
Find a care job
Explore flexible care job opportunities near you. Join our network of trusted Carer and start making a difference today. Live-in,overnight and hourly care roles available.
Why become a Curam Carer?
Discover the benefits of joining Curam as a Carer. Enjoy flexible work, fair pay, direct client relationships, and full control over your schedule.
Earnings calculator
Estimate your potential earnings as a Curam Carer. Use our simple calculator to see how much you can earn based on your availability and care type.
Become a registered Carer
Join Curam as a self-employed Carer. Set your own rates, choose your hours, and build meaningful relationships with clients across the UK.

 Vetted & approved carers
Vetted & approved carers
 DBS checked & insured
DBS checked & insured